| UW MSK Resident Projects |
|
|
|
|
Common Traumatic Injuries of the Pediatric ElbowPrint-friendly version of this pagePosted by daeheebang@hotmail.com, 12/6/03 at 7:46:22 PM.
Common Traumatic Injuries of the Pediatric Elbow First, we will review some basic concepts necessary to evaluate traumatic injuries of the pediatric elbow. Then, we will cover the most common injuries that you are likely to encounter in this population and discuss the incidence, mechanism of injury, diagnosis and treatment for these injuries.
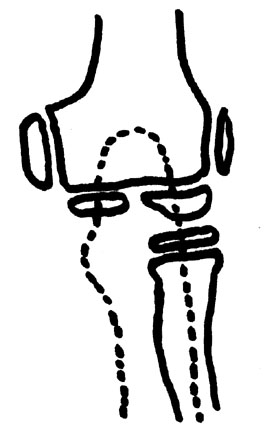
Ossification Centers of the Elbow Knowledge of the order and ages of appearance of the ossification centers of the elbow is essential in differentiating fractures from normal ossification centers in the pediatric elbow. A simple mnemonic, CRITOE, can be used to remember the sequence of appearance. Ossification centers - Approximate age of appearance Capitellum - 1 year Radial head - 5 years Internal epicondyle (Medial epicondyle) - 7 years Trochlea - 10 years Olecranon - 10 years External epicondyle (Lateral epicondyle) - 11 years Note: Females tend to have an earlier appearance of ossification centers by 1-2 years.
Diagram - The ossification centers of the elbow
Radiograph demonstrating ossification centers
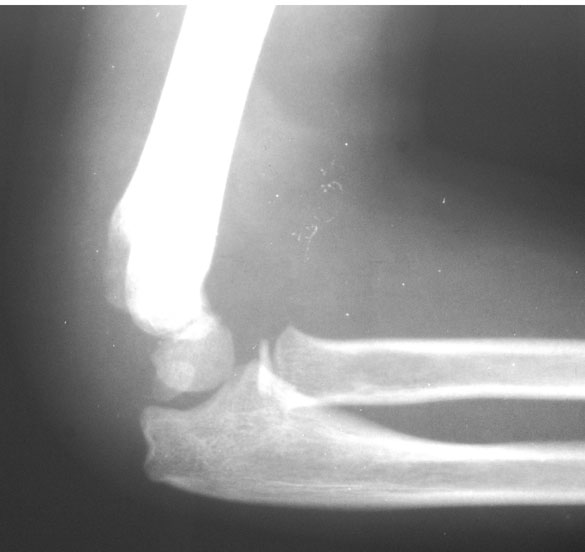
Fat Pad Sign There are two fat pads within the elbow which are helpful clues in the evaluation of traumatic injuries of the elbow. Normally, on a lateral radiograph of the elbow, the anterior fat pad is seen as a small triangular lucency anterior to the distal humeral diaphysis. The posterior fat pad is ordinarily not visualized on a lateral radiograph because it is tucked away in the olecranon fossa. With fractures, the joint becomes distended with blood. The anterior fat pad becomes displaced superiorly and outward from the humerus giving the so called "sail sign." The posterior fat pad gets displaced out of the olecranon fossa and becomes visible on the lateral radiograph. However, the fat pad sign can be seen with any joint effusion, making clinical history essential in the evaluation. In the setting of trauma, effusions are indicative of fractures about the elbow.
Radiograph - Radial head fracture with fat pad sign
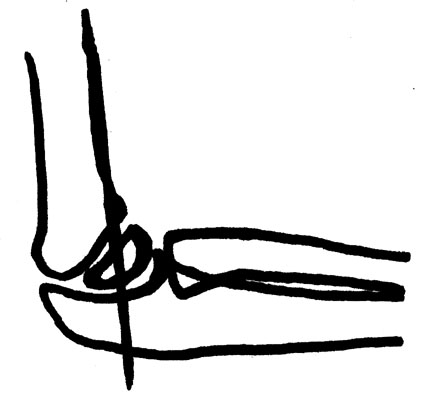
Common Fractures Supracondylar Fracture Supracondylar fractures make up 60% of all fractures about the elbow in the pediatric population. There are two types of supracondylar fractures based on the mechanism of injury. Of those, 96% are extension type fractures and 4% are flexion type fractures. We will discuss the extension type injury as it is, by far, the more common. These injuries are usually seen in skeletally immature patients in the first decade of life. The extension type fracture is caused by a fall on the outstreched hand with the elbow hyperextended. The distal fragment of the humerus will angulate and displace posteriorly, depending on the severity of the trauma. There is a relatively high risk of nerve injury (approximately 10% of fractures) associated with this injury. When there is nerve injury, the radial nerve is most commonly involved followed by the median nerve, and then the ulnar nerve. Radiological evaluation of these fractures can be difficult depending on the amount of displacement. The use of the fat pad sign is very helpful. Additionally, one should look for the anterior humeral line intersection with the capitellum. The anterior humeral line is drawn along the anterior humerus on a true lateral radiograph. Normally, this line intersects the middle third of the capitellum. In supracondylar fractures, the line often intersects the anterior third of the capitellum or beyond.
Diagram - The anterior humeral line
Radiograph - Supracondylar fracture with fat pad sign and displaced anterior humeral line Treatment depends on the amount of angulation or displacement that is present. In most non-displaced fractures, patients are immobilized for approximately three weeks and reassessed. However, depending on the amount of angulation, the patient may require reduction and percutaneous fixation. In completely displaced fractures, closed reduction with percutaneous pinning is the most common treatment option. Lateral Condyle Fracture Lateral condyle fractures are the second most common fractures about the elbow in the pediatric population, encompassing approximately 15% of fractures. Two mechanisms of injury have been proposed. First, the injury may result from a fall on the outstretched hand with the forearm supinated which transmits a force through the forearm extensor musculature to its attachment on the lateral condyle. These fractures may also occur with a force directed to the outstretched hand with the elbow flexed. The fracture can be easily identified radiographically if the capitellum is well ossified and displaced. In more difficult cases, oblique radiographs may assist in the diagnosis.
Radiograph - Fracture of lateral condyle Nondisplaced fractures may be treated by immobilization for approximately three weeks. However, frequent radiographs must be obtained to ensure that the fracture does not displace during the immobilization. To insure that the fracture does not displace, closed pinning of the fracture may be performed. Anatomic reduction is essential in these fractures because they are intra-articular and involve the growth plate. Therefore, displaced fractures are usually treated with open reduction and internal fixation. Medial Epicondyle Fracture Medial epicondyle fractures are the third most common fracture about the elbow in the pediatric population encompassing approximately 10% of fractures. These are typically seen in an older age group, most commonly adolescent males. This injury results from a valgus force combined with contraction of the forearm flexor muscles. If the valgus force is great enough, elbow dislocation can result, in addition to avulsion of the medial epicondyle. Radiographic diagnosis is not difficult in displaced fractures. In non-displaced fractures, the apophysis of the medial epicondyle may appear wider than normal. Comparison with the contralateral side will often be helpful in these situations. Additionally, some have recommended obtaining stress views to determine the stability of the elbow in these injuries.
Radiographs - Medial epicondyle fracture
Radiograph - Medial epicondyle fracture after reduction and pinning Treatment of this fracture depends on the amount of displacement of the epicondyle. Nondisplaced or minimally displaced fractures (<5 mm) can be treated with immobilization of the elbow and 90 degrees of flexion for approximately one week. Treatment of displaced fractures is controversial. If there is instability in addition to the fracture, open reduction and internal fixation is the treatment of choice. If there is no instability, these fractures can be treated with closed reduction. Proximal Radius Fracture This is the most common fracture about the elbow in adults. However, proximal radius fractures encompass only about 8% of fractures in the pediatric population. These fractures also differ from those seen in adults because they usually involve the radial neck and physis rather than the radial head, as in adults. These injuries can result from a fall on the outstretched hand with the elbow extended. In the skeletally immature, the force is transmitted through the head which is mostly cartilage, and directed to the physis and metaphysis. These fractures may also occur in association with posterior dislocation of the elbow. Displaced fractures are usually easily diagnosed on radiographs. However, non-displaced fractures can be difficult to visualize radiographically. Oblique views of the radius may be helpful.
Radiographs - Radial head fracture with fat pad sign The treatment of this fracture depends on the amount of angulation. In minimally angulated fractures, patients can be treated with immobilization in 90 degrees of flexion for approximately one week. With greater angulation, the fracture is treated with closed or percutaneous reduction. Open reduction is reserved for situations where closed or percutaneous reduction fails.
Other Traumatic Injuries of the Pediatric Elbow Dislocation of the Elbow Dislocation of the elbow is rare in children. The mechanism of injury is a posteriorly directed force. Closed reduction of the dislocation should be performed as soon as possible. First, any lateral displacement is corrected. Then, the arm is supinated and distal traction is applied with the patient's elbow flexed. Following reduction, the elbow is immobilized for 2-3 weeks. Radial Head Dislocation Isolated dislocation of the radial head is extremely rare. In the pediatric population, it is most likely due to bending of the ulna. Most dislocations of the radial head are associated with a fracture of the ulna, the Monteggia fracture-dislocation injury.
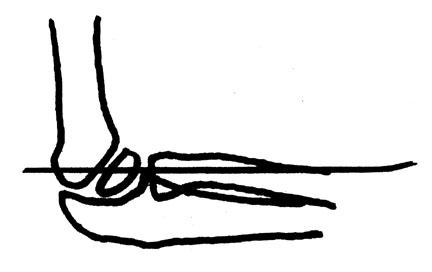
Radiographs - Monteggia fracture-dislocation injury Diagnosis can be made on lateral radiograph by examination of the radiocapitellar line and its intersection with the capitellum. The radiocapitellar line is created by bisecting the proximal radial shaft. This line normally intersects the capitellum in all radiographic projections. If it does not, the radial head is subluxed or dislocated. Radial head dislocations are treated with reduction.
Diagram - The radiocapitellar line
Radiographs - Dislocation of the radial head
Subluxation of the Radial Head This is the most common traumatic injury of the elbow in children. It is also known as "pulled elbow" or "nursemaid's elbow." The average age of incidence is 2-4 years. As children get older, the annular ligament gets thicker and resists tearing, making this injury less likely. The injury results from a pull on the extended pronated arm. The annular ligament tears at its attachment to the radius and the radial head moves distally. As the traction is relieved, the annular ligament gets caught between the radial head and the capitellum. The diagnosis is a clinical one. Radiographs can be obtained to rule out other injuries. Treatment entails reduction of the subluxation by forcefully supinating the forearm with the elbow flexed 60 to 90 degrees. The child should be observed following reduction as he/she should use the arm shortly after the subluxation is reduced. |
|